Although farriery overtly deals with the structures of the hoof capsule, a farrier may be involved with soft tissue injuries of the limb at any stage — from identification through rehabilitation. The term “soft tissue” technically includes any tissue that is not bone or horn: nerve, blood vessels, skin, subcutis, muscle, tendon, ligament, joint capsule, bursa, cartilage or fat.
While farriery can play a significant role in joint function, for now, synovial structures will be left for another time.
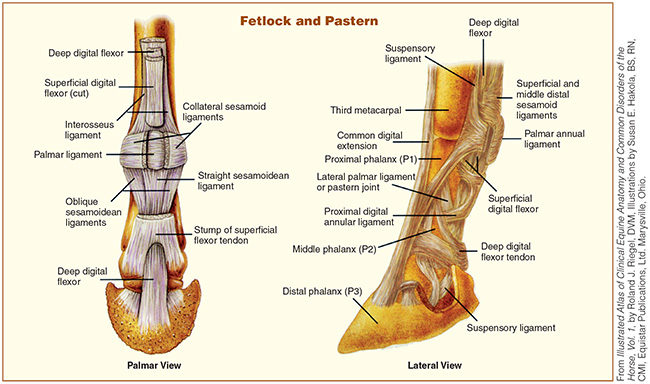
For the purposes of this article, the term “soft tissue injury” will be used in discussion of damage to the tendons and ligaments of the lower limb, with a focus on the deep digital flexor tendon (DDFT), superficial digital flexor tendon (SDFT), suspensory ligament (SL), impar ligaments and collateral sesamoidean ligaments(CSL).
What, Where And How
When considering any injured tissue and both the causes of the injury and the requirements for rehabilitation, it is useful to review the anatomy and mechanics behind the related structures.1
Tendons and ligaments are both fibrous connective tissues with similar functions in contributing to stability and movement of the musculoskeletal system. However, while ligaments join bone to bone or tendon to bone, tendons connect muscle to bone. Think of ligaments as stabilizing cables or guy lines, while tendons are the ropes connected to the pulleys and winches.
As a cable or rope can fray gradually due to repeated wear, or snap under sudden, overwhelming strain, soft tissue injuries can occur under low-grade, repeated stress, or as the result of a single incident. When the load upon a structure overwhelms the capacity of the structure, injury occurs. InAdams & Stashak’s Lameness in Horses, Laurie R. Goodrich, DVM, Ph.D., Dipl ACVS, writes, “Three types of injury may occur in tendons and ligaments: excessive strain, physical tearing, and percutaneous injury.”2
DDFT: The deep digital flexor tendon originates from the deep digital flexor muscle at the palmar (back) aspect of the forearm in the front leg. In the hind limb, the DDFT originates in the gaskin from the three heads of the deep digital flexor muscle. The DDFT runs along the palmar (or plantar) aspect of the lower limb, over the navicular bursa and attaches onto the flexor surface of P3. As implied by the name, contraction of the DDF muscle, and consequently tendon, acts to flex the leg.
SDFT: The superficial digital flexor tendon arises, as one might expect, from the superficial digital flexor muscle. The SDFT branches in two just below the fetlock. These branches insert onto the proximal region of P2. Contracture of the SDF muscle then exerts an upward force upon the palmar aspect of P2.
SL: The suspensory ligament (intraosseous muscle) lies at the palmar aspect of the limb. It originates at the distal row of carpal bones and the proximal end of MC3 (cannon bone). It runs down the leg in the metacarpal groove — the space created by the splint bones and the back of the cannon bone. Extensor branches of the suspensory ligament run from the sesamoid bones of the fetlock, around the front of the pastern, and down, meeting the common digital extensor tendon at the distal end of P1. Thus, upward force upon the SL (such as with heel elevation) may actually increase tension upon the SL
Collateral Sesamoidean Ligaments: Collateral Sesamoidean (suspensory navicular) ligaments begin from the distal end of P1, heading distally, crossing the pastern joint then dividing into branches. One branch of each ligament attaches to the navicular bone, the other to the opposing ligament.
Impar Ligament: The distal sesamoidean impar ligament is a fibrous sheet, extending from the distal border of the navicular bone to the DDFT.
Extensor Tendons: The extensor tendons (common digital extensor in the front limbs and long, lateral digital extensors in the hind) run down the front of the leg from their corresponding muscles in the forearm and gaskin respectively to insert onto the extensor process of P3. As the name implies, contracture of the extensor muscles and the corresponding shortening of tendons produces extension of the lower limb.
Biomechanics Review
It is important to bear in mind that no one structure acts alone within the body and that the principles of physics apply to a biological machine just as they do to a mechanical apparatus. Understanding the biomechanical forces at work within the foot and limb is critical to effective farriery. Any change to the foot will affect the forces upon the foot and upon the structures of the limb.

Ultrasound examinations, like this one being conducted at Rood and Riddle Equine Hospital in Lexington, Ky., can often help pinpoint soft-tissue injuries that might not be detectable in a radiograph.
When the limb is weight bearing, the joints are stabilized by limiting passive flexion through the opposing tensions of the DDFT, digital extensor tendons and collateral ligaments.3 During the propulsive phase, tightening of the DDFT places pressure upon the navicular bone, elevates the fetlock and extends the coffin joint.4
The forces that would act to hyperextend the joints of the foot and fetlock (the ground reaction force and downward weight of the horse) are counteracted by the stabilization of the suspensory apparatus (SL, intersesamoidean ligament and distal sesamoidean ligaments), upward force of the digital flexor tendons and the collateral ligaments of the joints.5
Disruption to, or excess strain upon any given structure, can alter this balance. Conversely, therapy of an injured structure is aimed at reducing the strain upon that structure by altering the forces upon it. However, it is important to remember that as the tendon or ligament heals, the goal is to eventually return the angles and load to normal so as not to adversely impact other structures.
According to Scott Morrison, DVM, head of the Podiatry Unit at Rood & Riddle Equine Hospital, Lexington, Ky., the degree of supportive farriery for a soft-tissue injury should take several factors into account: “the type of footing, degree of lameness, size of the injury, and exercise.”
“It depends on the lesion, and how the hoof capsule responds,” adds Morrison. “Once the horse is healed, you don’t want it still in that shoe.”
Enter, The Farrier
So, what is the farrier’s role in dealing with a soft tissue injury? Ideally, the farrier will play a role in everything from prevention of some injuries in the first place, to assistance with identifying a problem, to being a part of the therapeutic and rehabilitation efforts.
Before: Prevention
Farrier and lameness consultant Blake Brown claims that in 41 years of farriery, “over 85% of the lamenesses (I saw) were because the horse was not properly balanced to its individual conformation.”
The Penryn, Calif., shoer adds, “So much soft tissue damage is due to improper posterior and anterior hoof angles. Obviously some is happening in performance, but horses are conditioned to do their jobs. Still, when you continually see the same kind of injuries and see the angles, you start to realize that it’s a shoeing issue.”
The literature appears, for now at least, to support this assertion. At least one study has found that decreasing heel angle (as with underrun heels) is correlated to incidence of suspensory apparatus failure in racehorses.6
Morrison concurs, saying, “A dysfunctional foot may cause injury due to abnormal landing.” He urges equine professionals to “consider foot involvement in injury.”
During: Recognition And Treatment
The farrier is often the first equine professional to be presented with a lame horse. Additionally, given the frequent access to clues such as shoe and paddock wear, an observant farrier is ideally positioned to pick up on subtle signs of injury that may be eluding even the owner.
According to Morrison, some subtle signs that may indicate low-grade or gradual damage to tendon or ligament structures include: forging, interference, gait abnormalities, uneven wear patterns on shoes, stumbling, refusal to jump, refusal to land on the correct lead or stiffness in one direction.
Regarding shoe wear, Morrison stresses the importance of looking at both the ground surface and the hoof surface and at the wear from both heel-to-toe and medial-to-lateral.
Brown and Morrison agree on the implications of shoe wear, and the farrier adds the presence of holes in the paddock (from a horse attempting to unload structures itself) to the list.
Brown comments that an experienced, aware farrier can recognize lameness issues even before the owner. To the more subtle signs, he adds that while it is normal for the toe of the shoe to wear on the leading edge of the web (normal breakover), if the toe of the shoe is worn more than half way though the web in a normal shoeing cycle, it may indicate that the horse is having issues in the rear of the foot on the front feet and perhaps the hocks on the rear feet. Brown also points to shoe boils as a possible sign that the horse has a navicular problem.
“They lay down and curl their hoof up as tightly as they can to relieve the DDFT,” he says.
More blatant signs of soft tissue injury (usually acute injury) include: swelling and heat through the tendon sheath, significant or even non-weight-bearing lameness. Horses with an injury to the SDFT, DDFT, or SL will often toe touch and may be painful to palpation over the affected area. CSL damage can result in distortion above the coronary band on the affected side.7 Any of these signs signal the need for a further evaluation by a veterinarian.
Common injuries that may be indicated by these signs include: tendonitis or tearing of the DDFT or SDFT; desmitis of, or tears to, the SL or CSL; or tenosynovitis of the flexor tendon sheath.
After: Rehab Role
The farrier is an integral part of the rehabilitation team for these conditions. The major goals for therapy of a damaged tendon or ligament include:
- Reducing strain upon the tendon or ligament involved
- Avoiding retraction and thickened scarring of the involved structure that could pre-dispose it to re-injury.8
According to Denoix, et al,9 “A specific corrective shoeing program can be set up for each type of bone, tendon, and ligament (injury) in the equine foot according to:
- The precise nature of the structure involved,
- The evolution stage of the lesion and repair process.”
Because each structure has a different function and because different biomechanical forces act upon each structure, therapeutic farriery must be approached with these differences in mind. Morrison reiterates the concept that the goal in handling a soft-tissue injury is “to take tension off of the injured structure.” This can be achieved in a number of ways.

Lameness consultant and longtime farrier Blake Brown, shown examining a hoof, believes paying attention to posterior and anterior hoof angles as part of balancing a horse to its conformation can help prevent many soft-tissue injuries.
Unilateral injuries can be handled by flotation, keeping the injured side of the foot from sinking into the ground — by using wider branches on the affected side or through the use of extensions. With a severe injury to the DDFT, wedging of the heels and/or rolling of the toes may be recommended in order to take tension off of the tendons while the horse is walking. However, for SL or SDFT injuries, heel wedging is generally not thought to be indicated, as elevating the heels may put more tension on these structures.
Morrison emphasizes that implementation of these principles depends upon many factors. The deformability of the footing will alter the depth to which the foot sinks, and therefore the forces upon it. “On pavement, a wide branch may not be necessary,” he says, adding, “When returning to work, the horse may need more support. It depends on the lesion and how the hoof capsule responds.”
Morrison stresses the importance of remaining aware of the health of the hoof while implementing a shoeing protocol.
“The worse shape the hoof is in, the more risk to the structures above it.” Morrison notes that for horses with crushed or underrun heels, “layup may be an opportunity to pull the shoes and let the hoof capsule heal.”
The Therapeutic Team
Communication between owner, farrier and veterinarian is critical to the successful rehabilitation of any limb injury. The farrier may see the horse more frequently during the rehabilitation process than the veterinarian and can alert the owner to changes that may indicate that recovery is not progressing as expected. Besides noting abnormal wear to the shoe, Morrison suggests monitoring changes to the hoof capsule.
“It’s important to pick up on mild capsule changes,” he says. “First the wall gets a little vertical on the side of the greatest load and a flare to the side that is less loaded.”
The team must work together, not just in the rehabilitation phase, but also ideally throughout the entire process. This includes identifying a soft-tissue injury, as well as formulating a plan, treating and monitoring it.
“There’s no reason that if you’re dealing with an injury, that everyone can’t work together. The horse needs it,” says Brown.
Brown recommends that both veterinarians and farriers set professional egos aside for the good of the horse. “I never had problems in the city stopping to ask for directions. If people set everything else aside and said ‘I can learn something,’ then we’d have fewer problems.”
Morrison agrees on the need for a collaborative approach.
“The best case is if the vet keeps the farrier involved all along and goes into the mechanics of what is needed,” he says.
Morrison suggests if possible, farriers should have the veterinarian “give an idea of what you’re trying to accomplish — what structures to load and unload.” In a best-case scenario, Morrison says, the farrier would be present at the initial ultrasound imaging. (See “Diagnostic Techniques,” on Page 16.) Viewing the ultrasound helps everyone understand the structural damage. “The degree of therapeutic shoeing should match the degree of the lesion,” says Morrison. “Good communication saves trouble down the road.”
To repeat Brown’s point, “The horse needs it.”
Learn More
Why Equine Bones Break and Tendons Rupture
Understanding anatomy and physics can help prevent severe injuries.







Post a comment
Report Abusive Comment