Fescue lameness (also known as fescue foot) resembles ergotism (ergot poisoning); however, they are two different types of fescue toxicities.
Ergotism is a worldwide disease caused from ingestion of sclerotia (compact hardened mass of fungal mycelium) of the parasitic fungus Claviceps purpurea, which replaces the grain, seed of rye, or other forage plants such as bromes, bluegrasses, fescues and ryegrasses. Ergot infected pastures and hay made from ergot infected grasses is equally toxic. The sclerotia can be seen as elongated, hard, round projections about 5-10 mm long, brown to black in color with a white interior when they are broken open.
Fescue lameness, which resembles ergot poisoning, is believed to be caused by ergot alkaloids, especially ergovaline, produced by the endophyte fungus Neotyphodium coenophialum in tall fescue grass (Lolium arundinaceum, formerly Festuca arundinacea). Ergovaline has actions similar to those produced by sclerotia of Claviceps purpurea. However, ergotism is not the cause of fescue lameness.
Ergotism is most prevalent in late summer when the seed heads of grass mature. Fescue lameness is most common in late fall and winter. For control of these fescue toxicity diseases, all infected forage should be removed and destroyed.
Laboratory testing can be done for ergovaline (the ergot alkaloid of fescue lameness) and lolitrem B (the ergot alkaloid of perennial rye grass) in the feed, grain and hay samples collected. Choose a laboratory that uses High Performance Liquid Chromatography (HPLC) methodology. Thin layer chromatography (TLC) is not sensitive enough to identify ergot alkaloid levels less than 1 ppm. Ergovaline content of infected tall fescue often ranges from 100 to 500 ppb and less than 200 ppb is considered a toxic concentration. Removal of animals from infected fescue pasture reduces urinary ergovaline below detectable concentrations within 48 hours. Pregnant mares are especially sensitive and their progestogen levels can be monitored for exposure to ergot alkaloids.
Fescue toxicity causes vasoconstriction by direct action on the muscles of the arterioles (small branch of the artery leading into the capillaries) and repeated intake injures the vascular endothelium (single layer of cells lining the blood vessels). These actions initially reduce blood flow and eventually lead to complete stasis (inactivity) with terminal necrosis of the extremities due to thrombosis (blood clot). A cold environment predisposes the extremities to gangrene. Pregnant mares are sensitive to agalactia (failure to produce milk) and pregnancy abnormalities.
In both cases of fescue toxicity, lameness will begin in the ears, tail and one or both hind feet. The tail and ears may be affected with necrosis and gangrene. Low environmental temperature may also exacerbate the lesions of fescue toxicity. The toxin appears to be a vasoconstrictor acting as an agonist on blood vessels; this promotes hyperthermia in hot weather and results in cold extremities during cold weather. Erythema (redness of the skin caused by increased blood flow) and swelling of the coronary band area will often be seen in the hind limbs first. There is progressive lameness, anorexia (loss of appetite), depression and later, sloughing of hind hoof capsules; and dry gangrene (has no pus) of the hind distal phalanx (coffin bone) that causes them to separate from the distal interphalangeal joint (coffin joint) and descend out the hoof capsule.
Signs usually develop within 3 weeks after consuming contaminated fescue and the extent of involvement of a limb and the number of limbs affected depends on the daily intake. Body temperature, pulse and respiration rates are increased, as well.
Veterinary treatment involves dealing with the symptoms caused by the toxic event. Farrier treatment involves dealing with the hoof related problems that usually involves hoof sloughing, distal phalanx detachment and other secondary complications. Respectively, both professionals will have to deal with the hoof sloughing, distal phalanx detachment and dry gangrene of the distal phalanxes.
Over the years, I have dealt with many ergotism and fescue lameness ponies, donkeys and horses, although never a draft horse. When caught early enough, there may be little secondary complications. Many cases I am involved with have progressed into severe hind lameness, erythema, hoof capsule sloughing, distal phalanx detachment and dry gangrene of the distal phalanx(es). One of those case studies concerning a Michigan Mediterranean miniature donkey was published in American Farriers Journal (May/June, 2006; Pages 93-97). The donkey is still alive and sound to this day.
For both the veterinarian and the farrier, it is important to remember that many of these cases can survive and live a long, comfortable life. Many of the pleasure horses I have dealt with are even able to be ridden without any issues. One of the questions that arises is how the other phalanxes stay in the hoof capsule without falling out through the bottom of the foot. The simple answer is there are too many ligaments and tendons that prevent this from happening. Too many times these animals are euthanized due to misdiagnosing or lack of experience with dealing with these cases.
Below are some pictures of a recent case I dealt with in Lafayette, Ind., with Heather Darby Baker, a veterinarian at Wildcat Valley Animal Clinic.
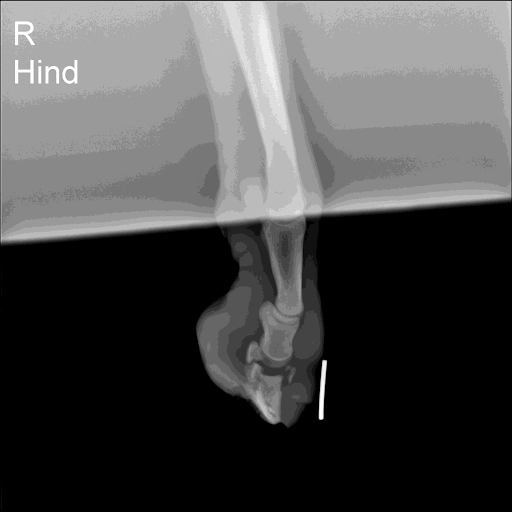
A radiograph of Orrie's right hind, which shows
a detached distal phalanx that is descending out
of the bottom of the sole.

A radiograph of Orrie's left hind showing an
attached distal phalanx with some remodeling
occurring.

Orrie's right hind before cleaning and trimming.

Orrie's right hind foot after cleaning and trimming.

Orrie's right hind distal phalanx was loose,
so it was removed with a Rogers clamp.

Orrie's right hind distal phalanx
after it was cleaned.

Orrie's right hind hoof 2 days after the removal
of the distal phalanx.

Orrie's right hind 1 month later shows the sole
growing back.

Orrie walking along at his home in Battle Ground, Ind.
References
- Amend KS, Bailey CS, Banse H, Baratt RM, Barger A, Barton MH, Bassage LH, Beerntsen BT, Bertone AL, Birks EK, Bischoff K, Blissitt K, Bonagura JD, Bourgeois M, Brown JA et al. 2012. Section 1: Diseases and Disorders. Ergot Related Toxicosis. Clinical Veterinary Advisor: The Horse. WB Saunders. pp. 175-178.
- Bacon CW. Fungal endophytes, other fungi, and their metabolites as extrinsic factors of grass quality. In: Forage Quality, Evaluation and Utilization. Nutrition Conference on Forage Quality, University of Nebraska, 1994: pp. 318-366.
- Brendemuehl JP, Williams MA, Boosinger TR, Ruffin DC. Plasma progestagen, tri-iodothyronine, and cortisol concentrations in postdate gestation foals exposed in utero to the tall fescue endophyte Acremonium coenophialum. In: Equine Reproduction VI. Biology Reprod Mono 1, 1995:pp. 53-59.
- Evans TJ, Blodgett DJ, Rottinghaus GE. 2012. Chapter 87-Fescue toxicosis. Veterinary Toxicology (Second Edition). Academic Press. pp. 1166-1177.
- Lacey J. Natural occurrence of mycotoxins in growing and conserved forage crops. In: Mycotoxins and Animal Foods. CRC Press, Inc., Florida, 1991: pp. 363-397.
- Osweiler, GD. 2014. Merck Veterinary Manual. Ergotism. Retrieved from merckvetmanual.com/toxicology/mycotoxicoses/ergotism?query=er
- gotismLastfull
- Osweiler, GD. 2014. Merck Veterinary Manual. Fescue Poisoning. Retrieved from merckvetmanual.com/toxicology/mycotoxicoses/fescue-poisoning
- Riet-Correa F, Mendez MC, Bergamo PN, Flores WN. Agalactia, reproductive problems and neonatal mortality in horses associated with the ingestion of Claviceps purpurea. Australian Vet. J. 1988 ; Vol 65, 6:192-193.
- Wright RG, Kenney D. Examining the mare's placenta and keeping foaling records. Ontario Ministry of Agriculture, Food and Rural Affairs, Guelph, Ontario. April 2001.
Learn More
- You Can't Keep a Good Donkey Down: Case study of an unusual animal that seems to be thriving despite losing her coffin bone.








Post a comment
Report Abusive Comment