In the medical community, ringbone is termed phalangeal exostosis. Simply put, it’s new bone growth on the proximal, middle or distal phalanx. This growth usually forms on the dorsal, dorsolateral and/or dorsomedial surfaces of the first and second phalanges and the extensor process of the third phalanx.
Unfortunately, ringbone may result in osteoarthritis or ankylosis (immobilization) of the pastern (proximal interphalangeal) or coffin (distal interphalangeal) joints.
Ringbone can be classified into four categories by the location of the new bone growth:
High Ringbone
New bone growth occurs on the distal end of the first phalanx or the proximal end of the second phalanx (Figure 1). Clinically, there will be a bulging of the tissues approximately 1 inch above the coronary band.
Low Ringbone
New bone growth occurs on the distal end of the second phalanx and the proximal end of the third phalanx (Figure 2). Radiographically, this may be especially prominent at the extensor process of the distal phalanx.

FIGURE 1 - High Ringbone
Periarticular Ringbone
New bone growth occurs around the joint capsule, but doesn’t involve the joint surface itself (Figure 3).
Articular Ringbone
New bone growth involves the joint surface of the pastern or coffin joints (Figure 4). In this classification, the new bone growth is also accompanied radiographically by osteophytes (outgrowths) depicting degenerative joint disease.
Ringbone is often described with a combination of these classification terminologies. Examples of these descriptive terms include articular high ringbone, periarticular high ringbone, articular low ringbone and periarticular low ringbone.

FIGURE 2 - Low Ringbone
Etiology
The most common etiology (cause) of ringbone is trauma. This can be the result of strain on the collateral ligaments, strains on the joint capsule attachments to the bone, wire cuts that invade the periosteum and direct blows to the tissues caused by things such as constantly hitting fence rails.
Conformational problems can also be responsible for strains and excessive trauma to the tissues. These conformational challenges predispose the animal to excessive strains on the collateral ligaments, joint capsule and tendon insertions.
When the animal is base-narrow and toes in or out, an excessive amount of strain is placed upon the lateral surfaces of the joints. When the animal is base-wide and toes in or out, there is an excessive strain on the medial surfaces. Prolonged, unbalanced shoeing can exaggerate these conditions or even be the primary cause.

FIGURE 3 - Periarticular Ringbone
Ringbone can also be caused by a fracture within the phalanges. These fractures may lead to an osteoarthritis of the pastern joint, which can develop into severe ringbone. When a fracture occurs within the extensor process of the distal phalanx, the healing process may result in a large, low ringbone.
Buttress foot is the common term for the damage that occurs from a strain on the insertion of the common digital extensor tendon, but the extensor process of the distal phalanx does not break. This strain results in a periostitis that causes new bone growth (low ringbone).
Clinical Signs
Lameness may or may not be present depending on the type of ringbone present. Initially, there might be swelling that develops into palpable heat and pain.
Periarticular ringbone may not exhibit any form of lameness, and rest will resolve any heat and swelling present in the tissues. Articular ringbone will result in a chronic lameness with some degree of swelling, heat and pain. When the animal is lunged in a tight circle, the lameness is usually amplified.
High ringbone that involves the proximal end of the second phalanx may exhibit periodic swelling and lameness that is resolved by rest. As soon as the horse returns to work, however, these clinical symptoms reappear. When the joint is flexed, range of motion is noticeably reduced. Rotation of the phalanx will result in a painful response. These animals tend to move like laminitic horses—the heel lands long before the toe.

FIGURE 4 - Articular Ringbone
Differential Diagnosis
Several other disorders should be kept in mind when a diagnosis of ringbone is being considered. These include fractures, osteochondritis dissecans (OCD) lesions, ligament desmitis and tendonitis.
Diagnosis
In the earliest stages of inflammation and new bone growth, infrared thermography will reveal increased thermal patterns along the dorsal and medial and/or lateral aspects of the pastern (Figure 5). This thermal pattern can be unilateral or bilateral in nature. Perineural anesthesia, such as a ring block, can be performed above the pastern to alleviate the lameness.
A definitive diagnosis can only be made through radiology, and it’s important to radiograph both pasterns for comparison. These films will show the extent of the damage and joint involvement and rule out OCD and fractures.

FIGURE 5. Infrared thermograph depicting increased thermal gradient on the dorsal surface of the pastern joint.
If soft tissue swelling is present and the infrared thermal gradients are increased over these anatomical areas, a tentative diagnosis of early ringbone can be made if a diagnostic nerve block relieves the lameness. The early diagnosis may offer treatment options that are not applicable when the case becomes chronic.
Ringbone lesions that can be observed radiographically are:
- Peripheral osteophytosis in the very early stages of articular ringbone.
- Periarticular new bone formation in the early stages of nonarticular ringbone.
- These two radiographic lesions become almost indistinguishable as the condition progresses.
- Diffuse subchondral bone lucencies can be seen at the distal end of the proximal phalanx.
Treatment
Even in the earliest detectable stages, ringbone cases have a guarded prognosis for a return to athletic endeavors. With aggressive physical therapy and a modified training schedule, nonarticular forms of ringbone have a better prognosis for return to serviceability than articular forms. Most cases of articular ringbone will progress to degenerative joint disease.
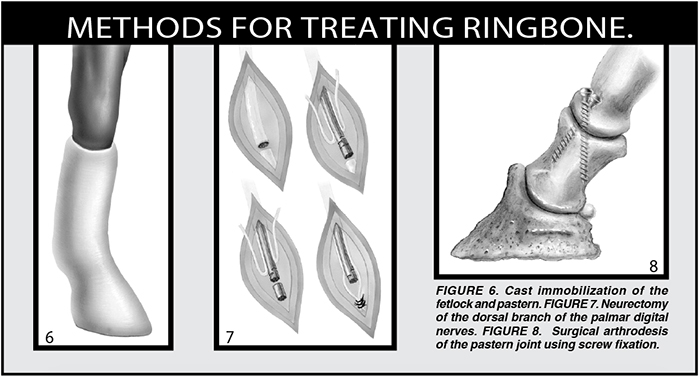
The following treatment regimes are fundamental in nature:
-
Early stages with almost nonexistent bone growth: Rest with joint movement limited by a Robert Jones bandage or light cast (Figure 6). Nutraceutical therapy, such as MSM (methylsulfonylmethane), glucosamine and chondroitin sulfate should complement the reduction in inflammation. Aggressive physical therapy modalities will yield excellent results at this stage. With these techniques alone, the soundness of the athlete should be maintained. Warm, moist heat and cold therapy will decrease the inflammatory reaction within these tissues. Low-level light therapy will increase the circulation within the tissues and keep the inflammatory reaction under control. All efforts should be made to reduce trauma to the area with proper shoeing and modification of the training technique and/or schedule.
-
Chronic cases that are periarticular: Systemic analgesics, rest, complementary nutraceutical therapy and possibly a dorsal digital neurectomy (Figure 7) should all be considered. Physical therapy techniques should always be utilized to reduce the inflammation in the tissues around the lesions. In severe cases, an arthrodesis of the joint should be considered (Figure 8).
-
High ringbone that is articular: Systemic and intra-articular therapies are essential to alleviate synovitis, capsulitis and generalized inflammation. Surgical arthrodesis of the proximal interphalangeal joint is the treatment of choice for a good prognosis in returning to work. If more than one joint is involved, then systemic and physical therapies are more desirable.
- Chronic cases that are articular: Surgical arthrodesis utilizing internal fixation and post-surgical casting are the treatments of choice.
Nearly all of these cases should be shod with a roller-motion shoe that will help reduce the action of the ankylosed or involved joints. Any complementary farrier technique that will reduce trauma to the tissues should be considered—an example would be using a rim pad and hoof cushion material.

FIGURE 9. Extensive new bone growth in a horse with both high and low ringbone.
Prognosis
When considering some forms of nonarticular ringbone, the prognosis is fair to good with early detection and aggressive treatment. When the ringbone is articular in nature, it invariably progresses to degenerative joint disease. These cases carry a very unfavorable prognosis for a return to the same level of athletic ability.
Surgical arthrodesis of the proximal interphalangeal joint will often allow soundness as a salvage operation, but not as an athletic restoration procedure. Low nonarticular ringbone carries a guarded prognosis and will often mechanically influence the gait even after the pain is gone.






Post a comment
Report Abusive Comment